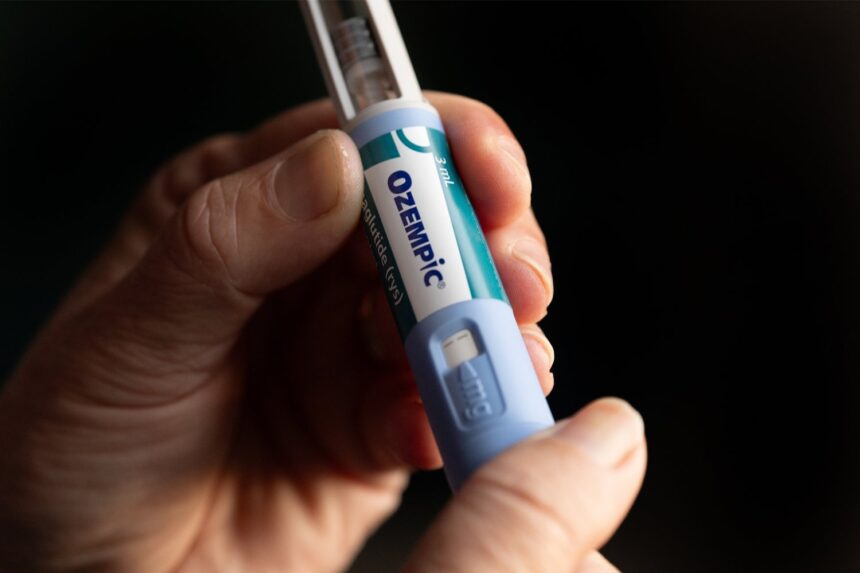
The advent of Ozempic, Wegovy, and other weight loss drugs could lighten people’s medical bills elsewhere. New research published this week shows that when people lose weight, their health care costs often decline along with it.
Researchers at Emory University conducted the study, which looked at health care spending among people either with private insurance or Medicare. They found that people who had lost as little as 5% body weight over a year’s time tended to spend less on health care. The findings could have major implications for assessing the value of newer, more effective weight loss medications, the researchers say.
While obesity isn’t necessarily unhealthy in of itself, it can raise the risk of many other health problems, including knee pain, type 2 diabetes, and obstructive sleep apnea. Previous research has suggested that these obesity-related conditions not only take a toll on our health, but our wallets. A 2021 study, for instance, estimated that obesity in the U.S. was associated with $260 billion in annual health care costs, as of 2016. While past studies have found that treating obesity can lower health care costs, the researchers say their new study provides a more expansive and updated analysis of these financial benefits.
They examined data from the Medical Expenditure Panel Survey–Household Component, a regularly conducted and nationally representative survey of Americans’ health-related spending. These surveys are conducted over a two-year period, which allowed the researchers to track how people’s spending may have changed following any substantial change in weight. The researchers specifically focused on Americans who had a body mass index over 25 (the cut-off for being overweight) and who had one or more of ten chronic conditions, eight of which are associated with obesity, such as type 2 diabetes or back pain. The researchers included 17,209 adults in their analysis, including more than 3,700 people who had Medicare.
Overall, the researchers estimated that people with private insurance who lost 5% body weight spent an average 8% less on their health care (about $670 in 2023 dollars), while people who lost 25% of their weight spent 34% less on health care (nearly $3,000). The savings were similar for people on Medicare percentage-wise, but higher in money saved due to their higher net costs. Medicare patients who lost 5% weight were estimated to spend an average $1,262 less (7%), while those who lost 25% weight spent an average $5,442 less (31%).
‘In this cross-sectional study, projected annual savings from weight loss among US adults with obesity were substantial for both Medicare and employer-based insurance,” the researchers wrote in their paper, published this month in JAMA Network Open.
The team’s findings do largely come from people who lost weight long before these newer GLP-1 drugs were even around. Ozempic was first approved as a diabetes drug in 2017, for instance, but it wasn’t widely prescribed off-label to treat obesity until after the approval of Wegovy in 2021 (both drugs are made with the same active ingredient semaglutide). What has made these medications so promising, however, is how reliable they are at helping people lose weight. In clinical trials, people have consistently lost more weight taking these medications compared to those taking a placebo, with an average weight loss ranging from 10% to 20% over a year’s time, depending on the specific drug. So it’s likely that the savings associated with weight loss could be even more profound on a population level nowadays, the researchers note.
Another important consideration is that Ozempic and similar drugs don’t come cheap, with list prices as high as over $1,000 a month. Much of this cost can be covered by people’s insurance, but many private insurance plans have limited their coverage of these drugs, while Medicare is explicitly banned from covering anti-obesity medications (people can sometimes be covered if the drug is prescribed to treat obesity-related conditions). These high prices obviously affect any discussion of their cost-effectiveness. At the same time, other studies have found that bariatric surgery can provide net savings in health care spending by effectively reducing obesity, despite also costing lots of money upfront (as much as $26,000 per patient). And the researchers note that they only looked at health care costs associated with people’s existing obesity-related conditions. Given that many people taking GLP-1 therapy today may avoid developing these conditions at all, the projected savings in health care could be even higher than their estimates, the researchers say.
“Improving access to new weight loss medications, along with existing evidence-based behavior change and weight loss interventions, should help reduce health care spending associated with obesity in the U.S.” they wrote.
It also isn’t just money that these drugs could be helping us save at the end of the day, but lives. A study earlier this year estimated that higher uptake of GLP-1 drugs could prevent 42,000 deaths annually in the U.S. from obesity- or diabetes-related health problems.
Read the full article here